Biomedical applications of electrical stimulation
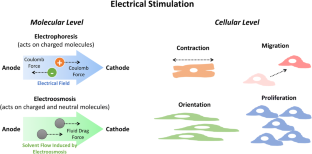
This review provides a comprehensive overview on the biomedical applications of electrical stimulation (EStim). EStim has a wide range of direct effects on both biomolecules and cells. These effects have been exploited to facilitate proliferation and functional development of engineered tissue constructs for regenerative medicine applications. They have also been tested or used in clinics for pain mitigation, muscle rehabilitation, the treatment of motor/consciousness disorders, wound healing, and drug delivery. However, the research on fundamental mechanism of cellular response to EStim has fell behind its applications, which has hindered the full exploitation of the clinical potential of EStim. Moreover, despite the positive outcome from the in vitro and animal studies testing the efficacy of EStim, existing clinical trials failed to establish strong, conclusive supports for the therapeutic efficacy of EStim for most of the clinical applications mentioned above. Two potential directions of future research to improve the clinical utility of EStim are presented, including the optimization and standardization of the stimulation protocol and the development of more tissue-matching devices.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save
Springer+ Basic
€32.70 /Month
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Buy Now
Price includes VAT (France)
Instant access to the full article PDF.
Rent this article via DeepDyve
Similar content being viewed by others

Electrical stimulation as a novel tool for regulating cell behavior in tissue engineering
Article Open access 05 December 2019

Biomaterials-enabled electrical stimulation for tissue healing and regeneration
Article Open access 21 May 2024
Stimulation strategies for electrical and magnetic modulation of cells and tissues
Article Open access 01 July 2023
References
- Gratieri T, Santer V, Kalia YN (2017) Basic principles and current status of transcorneal and transscleral iontophoresis. Expert Opin Drug Deliv 14(9):1091–1102. https://doi.org/10.1080/17425247.2017.1266334ArticleCASPubMedGoogle Scholar
- Balint R, Cassidy NJ, Cartmell SH (2013) Electrical stimulation: a novel tool for tissue engineering. Tissue Eng Part B Rev 19(1):48–57. https://doi.org/10.1089/ten.TEB.2012.0183ArticleCASPubMedGoogle Scholar
- Gordon T (2016) Electrical stimulation to enhance axon regeneration after peripheral nerve injuries in animal models and humans. Neurotherapeutics 13(2):295–310. https://doi.org/10.1007/s13311-015-0415-1ArticlePubMedPubMed CentralGoogle Scholar
- Love MR, Palee S, Chattipakorn SC, Chattipakorn N (2018) Effects of electrical stimulation on cell proliferation and apoptosis. J Cell Physiol 233(3):1860–1876. https://doi.org/10.1002/jcp.25975ArticleCASPubMedGoogle Scholar
- Ghasemi-Mobarakeh L, Prabhakaran MP, Morshed M, Nasr-Esfahani MH, Baharvand H, Kiani S, Al-Deyab SS, Ramakrishna S (2011) Application of conductive polymers, scaffolds and electrical stimulation for nerve tissue engineering. J Tissue Eng Regen Med 5(4):e17–e35. https://doi.org/10.1002/term.383ArticleCASPubMedGoogle Scholar
- Pedrotty DM, Koh J, Davis BH, Taylor DA, Wolf P, Niklason LE (2005) Engineering skeletal myoblasts: roles of three-dimensional culture and electrical stimulation. Am J Physiol Heart Circ Physiol 288(4):H1620–H1626. https://doi.org/10.1152/ajpheart.00610.2003ArticleCASPubMedGoogle Scholar
- Koning M, Harmsen MC, van Luyn MJ, Werker PM (2009) Current opportunities and challenges in skeletal muscle tissue engineering. J Tissue Eng Regen Med 3(6):407–415. https://doi.org/10.1002/term.190ArticleCASPubMedGoogle Scholar
- Bach AD, Beier JP, Stern-Staeter J, Horch RE (2004) Skeletal muscle tissue engineering. J Cell Mol Med 8(4):413–422. https://doi.org/10.1111/j.1582-4934.2004.tb00466.xArticleCASPubMedPubMed CentralGoogle Scholar
- Stoppel WL, Kaplan DL, Black LD 3rd (2016) Electrical and mechanical stimulation of cardiac cells and tissue constructs. Adv Drug Deliv Rev 96:135–155. https://doi.org/10.1016/j.addr.2015.07.009ArticleCASPubMedGoogle Scholar
- Victoria G, Petrisor B, Drew B, Dick D (2009) Bone stimulation for fracture healing: what’s all the fuss? Indian J Orthop 43(2):117–120. https://doi.org/10.4103/0019-5413.50844ArticlePubMedPubMed CentralGoogle Scholar
- Griffin M, Bayat A (2011) Electrical stimulation in bone healing: critical analysis by evaluating levels of evidence. Eplasty 11:e34 PubMedPubMed CentralGoogle Scholar
- Leppik L, Zhihua H, Mobini S, Thottakkattumana Parameswaran V, Eischen-Loges M, Slavici A, Helbing J, Pindur L, Oliveira KMC, Bhavsar MB, Hudak L, Henrich D, Barker JH (2018) Combining electrical stimulation and tissue engineering to treat large bone defects in a rat model. Sci Rep 8(1):6307. https://doi.org/10.1038/s41598-018-24892-0ArticleCASPubMedPubMed CentralGoogle Scholar
- Thakral G, Lafontaine J, Najafi B, Talal TK, Kim P, Lavery LA (2013) Electrical stimulation to accelerate wound healing. Diabetes Foot Ankle. https://doi.org/10.3402/dfa.v4i0.22081ArticleGoogle Scholar
- Zhao M, Song B, Pu J, Wada T, Reid B, Tai G, Wang F, Guo A, Walczysko P, Gu Y, Sasaki T, Suzuki A, Forrester JV, Bourne HR, Devreotes PN, McCaig CD, Penninger JM (2006) Electrical signals control wound healing through phosphatidylinositol-3-OH kinase-gamma and PTEN. Nature 442(7101):457–460. https://doi.org/10.1038/nature04925ArticleCASPubMedGoogle Scholar
- Zhao M (2009) Electrical fields in wound healing—an overriding signal that directs cell migration. Semin Cell Dev Biol 20(6):674–682. https://doi.org/10.1016/j.semcdb.2008.12.009ArticleCASPubMedGoogle Scholar
- Kroeling P, Gross A, Graham N, Burnie SJ, Szeto G, Goldsmith CH, Haines T, Forget M (2013) Electrotherapy for neck pain. Cochrane Database Syst Rev 8:CD004251. https://doi.org/10.1002/14651858.CD004251.pub5ArticleGoogle Scholar
- Sbruzzi G, Silveira SA, Silva DV, Coronel CC, Plentz RD (2012) Transcutaneous electrical nerve stimulation after thoracic surgery: systematic review and meta-analysis of 11 randomized trials. Rev Bras Cir Cardiovasc 27(1):75–87. https://doi.org/10.5935/1678-9741.20120012ArticlePubMedGoogle Scholar
- Hurlow A, Bennett MI, Robb KA, Johnson MI, Simpson KH, Oxberry SG (2012) Transcutaneous electric nerve stimulation (TENS) for cancer pain in adults. Cochrane Database Syst Rev 3:CD006276. https://doi.org/10.1002/14651858.CD006276.pub3ArticleGoogle Scholar
- Claydon LS, Chesterton LS (2008) Does transcutaneous electrical nerve stimulation (TENS) produce ‘dose-responses’? A review of systematic reviews on chronic pain. Phys Ther Rev 13(6):450–463 ArticleGoogle Scholar
- Nnoaham KE, Kumbang J (2008) Transcutaneous electrical nerve stimulation (TENS) for chronic pain. Cochrane Database Syst Rev 3:CD003222. https://doi.org/10.1002/14651858.CD003222.pub2ArticleGoogle Scholar
- Jin DM, Xu Y, Geng DF, Yan TB (2010) Effect of transcutaneous electrical nerve stimulation on symptomatic diabetic peripheral neuropathy: a meta-analysis of randomized controlled trials. Diabetes Res Clin Pract 89(1):10–15. https://doi.org/10.1016/j.diabres.2010.03.021ArticlePubMedGoogle Scholar
- Bjordal JM, Johnson MI, Lopes-Martins RA, Bogen B, Chow R, Ljunggren AE (2007) Short-term efficacy of physical interventions in osteoarthritic knee pain. A systematic review and meta-analysis of randomised placebo-controlled trials. BMC Musculoskelet Disord 8:51. https://doi.org/10.1186/1471-2474-8-51ArticlePubMedPubMed CentralGoogle Scholar
- Johnson M, Martinson M (2007) Efficacy of electrical nerve stimulation for chronic musculoskeletal pain: a meta-analysis of randomized controlled trials. Pain. 130(1–2):157–165. https://doi.org/10.1016/j.pain.2007.02.007ArticlePubMedGoogle Scholar
- Lake DA (1992) Neuromuscular electrical stimulation. An overview and its application in the treatment of sports injuries. Sports Med 13(5):320–336. https://doi.org/10.2165/00007256-199213050-00003ArticleCASPubMedGoogle Scholar
- Benninger DH, Lomarev M, Lopez G, Wassermann EM, Li X, Considine E, Hallett M (2010) Transcranial direct current stimulation for the treatment of Parkinson’s disease. J Neurol Neurosurg Psychiatry 81(10):1105–1111. https://doi.org/10.1136/jnnp.2009.202556ArticlePubMedPubMed CentralGoogle Scholar
- Fridriksson J, Rorden C, Elm J, Sen S, George MS, Bonilha L (2018) Transcranial direct current stimulation vs sham stimulation to treat aphasia after stroke: a randomized clinical trial. JAMA Neurol 75(12):1470–1476. https://doi.org/10.1001/jamaneurol.2018.2287ArticlePubMedPubMed CentralGoogle Scholar
- Ferrucci R, Vergari M, Cogiamanian F, Bocci T, Ciocca M, Tomasini E, De Riz M, Scarpini E, Priori A (2014) Transcranial direct current stimulation (tDCS) for fatigue in multiple sclerosis. NeuroRehabilitation 34(1):121–127. https://doi.org/10.3233/NRE-131019ArticlePubMedGoogle Scholar
- San-Juan D, Sarmiento CI, Gonzalez KM, Orenday Barraza JM (2018) Successful treatment of a drug-resistant epilepsy by long-term transcranial direct current stimulation: a case report. Front Neurol 9:65. https://doi.org/10.3389/fneur.2018.00065ArticlePubMedPubMed CentralGoogle Scholar
- Bystad M, Gronli O, Rasmussen ID, Gundersen N, Nordvang L, Wang-Iversen H, Aslaksen PM (2016) Transcranial direct current stimulation as a memory enhancer in patients with Alzheimer’s disease: a randomized, placebo-controlled trial. Alzheimers Res Ther 8(1):13. https://doi.org/10.1186/s13195-016-0180-3ArticlePubMedPubMed CentralGoogle Scholar
- Shekhawat GS, Vanneste S (2018) Optimization of transcranial direct current stimulation of dorsolateral prefrontal cortex for tinnitus: a non-linear dose-response effect. Sci Rep 8(1):8311. https://doi.org/10.1038/s41598-018-26665-1ArticleCASPubMedPubMed CentralGoogle Scholar
- Sampaio-Junior B, Tortella G, Borrione L, Moffa AH, Machado-Vieira R, Cretaz E, Fernandes da Silva A, Fraguas R, Aparicio LV, Klein I, Lafer B, Goerigk S, Bensenor IM, Lotufo PA, Gattaz WF, Brunoni AR (2018) Efficacy and safety of transcranial direct current stimulation as an add-on treatment for bipolar depression: a randomized clinical trial. JAMA Psychiatry 75(2):158–166. https://doi.org/10.1001/jamapsychiatry.2017.4040ArticlePubMedGoogle Scholar
- da Silva MC, Conti CL, Klauss J, Alves LG, do Nascimento Cavalcante HM, Fregni F, Nitsche MA, Nakamura-Palacios EM (2013) Behavioral effects of transcranial direct current stimulation (tDCS) induced dorsolateral prefrontal cortex plasticity in alcohol dependence. J Physiol Paris 107(6):493–502. https://doi.org/10.1016/j.jphysparis.2013.07.003ArticlePubMedGoogle Scholar
- Lefaucheur JP, Antal A, Ayache SS, Benninger DH, Brunelin J, Cogiamanian F, Cotelli M, De Ridder D, Ferrucci R, Langguth B, Marangolo P, Mylius V, Nitsche MA, Padberg F, Palm U, Poulet E, Priori A, Rossi S, Schecklmann M, Vanneste S, Ziemann U, Garcia-Larrea L, Paulus W (2017) Evidence-based guidelines on the therapeutic use of transcranial direct current stimulation (tDCS). Clin Neurophysiol 128(1):56–92. https://doi.org/10.1016/j.clinph.2016.10.087ArticlePubMedGoogle Scholar
- Panus PC, Campbell J, Kulkarni SB, Herrick RT, Ravis WR, Banga AK (1997) Transdermal iontophoretic delivery of ketoprofen through human cadaver skin and in humans. J Control Release 44(2):113–121. https://doi.org/10.1016/S0168-3659(96)01509-XArticleCASGoogle Scholar
- Labala S, Jose A, Venuganti VVK (2016) Transcutaneous iontophoretic delivery of STAT3 siRNA using layer-by-layer chitosan coated gold nanoparticles to treat melanoma. Colloids Surf B Biointerfaces 146:188–197. https://doi.org/10.1016/j.colsurfb.2016.05.076ArticleCASPubMedGoogle Scholar
- Bernardi DS, Bitencourt C, da Silveira DSC, da Cruz ELCM, Pereira-da-Silva MA, Faccioli LH, Lopez RFV (2016) Effective transcutaneous immunization using a combination of iontophoresis and nanoparticles. Nanomedicine 12(8):2439–2448. https://doi.org/10.1016/j.nano.2016.07.001ArticleCASPubMedGoogle Scholar
- Doucet BM, Lam A, Griffin L (2012) Neuromuscular electrical stimulation for skeletal muscle function. Yale J Biol Med 85(2):201–215 PubMedPubMed CentralGoogle Scholar
- Kern H, Carraro U, Adami N, Biral D, Hofer C, Forstner C, Modlin M, Vogelauer M, Pond A, Boncompagni S, Paolini C, Mayr W, Protasi F, Zampieri S (2010) Home-based functional electrical stimulation rescues permanently denervated muscles in paraplegic patients with complete lower motor neuron lesion. Neurorehabil Neural Repair 24(8):709–721. https://doi.org/10.1177/1545968310366129ArticlePubMedGoogle Scholar
- Johnson M (2007) Transcutaneous electrical nerve stimulation: mechanisms, clinical application and evidence. Rev Pain 1(1):7–11. https://doi.org/10.1177/204946370700100103ArticlePubMedPubMed CentralGoogle Scholar
- Tandon N, Cannizzaro C, Chao PH, Maidhof R, Marsano A, Au HT, Radisic M, Vunjak-Novakovic G (2009) Electrical stimulation systems for cardiac tissue engineering. Nat Protoc 4(2):155–173. https://doi.org/10.1038/nprot.2008.183ArticleCASPubMedPubMed CentralGoogle Scholar
- Feiner R, Engel L, Fleischer S, Malki M, Gal I, Shapira A, Shacham-Diamand Y, Dvir T (2016) Engineered hybrid cardiac patches with multifunctional electronics for online monitoring and regulation of tissue function. Nat Mater 15(6):679–685. https://doi.org/10.1038/nmat4590ArticleCASPubMedPubMed CentralGoogle Scholar
- Ahadian S, Ramon-Azcon J, Ostrovidov S, Camci-Unal G, Hosseini V, Kaji H, Ino K, Shiku H, Khademhosseini A, Matsue T (2012) Interdigitated array of Pt electrodes for electrical stimulation and engineering of aligned muscle tissue. Lab Chip 12(18):3491–3503. https://doi.org/10.1039/c2lc40479fArticleCASPubMedGoogle Scholar
- Koo J, MacEwan MR, Kang SK, Won SM, Stephen M, Gamble P, Xie Z, Yan Y, Chen YY, Shin J, Birenbaum N, Chung S, Kim SB, Khalifeh J, Harburg DV, Bean K, Paskett M, Kim J, Zohny ZS, Lee SM, Zhang R, Luo K, Ji B, Banks A, Lee HM, Huang Y, Ray WZ, Rogers JA (2018) Wireless bioresorbable electronic system enables sustained nonpharmacological neuroregenerative therapy. Nat Med 24(12):1830–1836. https://doi.org/10.1038/s41591-018-0196-2ArticleCASPubMedGoogle Scholar
- Xu B, Akhtar A, Liu Y, Chen H, Yeo WH, Park SI, Boyce B, Kim H, Yu J, Lai HY, Jung S, Zhou Y, Kim J, Cho S, Huang Y, Bretl T, Rogers JA (2016) An epidermal stimulation and sensing platform for sensorimotor prosthetic control, management of lower back exertion, and electrical muscle activation. Adv Mater 28(22):4462–4471. https://doi.org/10.1002/adma.201504155ArticleCASPubMedGoogle Scholar
- Lee HU, Blasiak A, Agrawal DR, Loong DTB, Thakor NV, All AH, Ho JS, Yang IH (2017) Subcellular electrical stimulation of neurons enhances the myelination of axons by oligodendrocytes. PLoS One 12(7):e0179642. https://doi.org/10.1371/journal.pone.0179642ArticleCASPubMedPubMed CentralGoogle Scholar
- Iwasa SN, Rashidi A, Sefton E, Liu NX, Popovic MR, Morshead CM (2019) Charge-balanced electrical stimulation can modulate neural precursor cell migration in the presence of endogenous electric fields in mouse brains. Eneuro. https://doi.org/10.1523/ENEURO.0382-19.2019ArticlePubMedPubMed CentralGoogle Scholar
- Hu M, Hong L, Liu C, Hong S, He S, Zhou M, Huang G, Chen Q (2019) Electrical stimulation enhances neuronal cell activity mediated by Schwann cell derived exosomes. Sci Rep 9(1):4206. https://doi.org/10.1038/s41598-019-41007-5ArticleCASPubMedPubMed CentralGoogle Scholar
- Gordon T, Amirjani N, Edwards DC, Chan KM (2010) Brief post-surgical electrical stimulation accelerates axon regeneration and muscle reinnervation without affecting the functional measures in carpal tunnel syndrome patients. Exp Neurol 223(1):192–202. https://doi.org/10.1016/j.expneurol.2009.09.020ArticlePubMedGoogle Scholar
- Gordon T, Sulaiman OAR, Ladak A (2009) Electrical stimulation for improving nerve regeneration: where do we stand?, Chapter 24. In: International review of neurobiology. Academic Press, pp 433–444
- Zeighami A, Alizadeh F, Saviz M (2019) Optimal currents for electrical stimulation of bone fracture repair: a computational analysis including variations in frequency, tissue properties, and fracture morphology. Bioelectromagnetics 40(2):128–135. https://doi.org/10.1002/bem.22173ArticlePubMedGoogle Scholar
- Portan DV, Deligianni DD, Papanicolaou GC, Kostopoulos V, Psarras GC, Tyllianakis M (2019) Combined optimized effect of a highly self-organized nanosubstrate and an electric field on osteoblast bone cells activity. Biomed Res Int 2019:7574635. https://doi.org/10.1155/2019/7574635ArticleCASPubMedPubMed CentralGoogle Scholar
- Su C-Y, Fang T, Fang H-W (2017) Effects of electrostatic field on osteoblast cells for bone regeneration applications. Biomed Res Int 2017:7124817. https://doi.org/10.1155/2017/7124817ArticleCASPubMedPubMed CentralGoogle Scholar
- Eischen-Loges M, Oliveira KMC, Bhavsar MB, Barker JH, Leppik L (2018) Pretreating mesenchymal stem cells with electrical stimulation causes sustained long-lasting pro-osteogenic effects. PeerJ 6:e4959. https://doi.org/10.7717/peerj.4959ArticleCASPubMedPubMed CentralGoogle Scholar
- Vadlamani RA, Nie Y, Detwiler DA, Dhanabal A, Kraft AM, Kuang S, Gavin TP, Garner AL (2019) Nanosecond pulsed electric field induced proliferation and differentiation of osteoblasts and myoblasts. J R Soc Interface 16(155):20190079. https://doi.org/10.1098/rsif.2019.0079ArticleCASPubMedPubMed CentralGoogle Scholar
- Nagamine K, Sato H, Kai H, Kaji H, Kanzaki M, Nishizawa M (2018) Contractile skeletal muscle cells cultured with a conducting soft wire for effective, selective stimulation. Sci Rep 8(1):2253. https://doi.org/10.1038/s41598-018-20729-yArticleCASPubMedPubMed CentralGoogle Scholar
- Naskar S, Basu B, Kumaran V. Experimental analysis of effect of electric field on mouse myoblast cells using high throughput microfluidic bioreactor. In: 10th World biomaterials congress, 17 May–22 May, 2016, Montréal
- Li L, Gu W, Du J, Reid B, Deng X, Liu Z, Zong Z, Wang H, Yao B, Yang C, Yan J, Zeng L, Chalmers L, Zhao M, Jiang J (2012) Electric fields guide migration of epidermal stem cells and promote skin wound healing. Wound Repair Regen 20(6):840–851. https://doi.org/10.1111/j.1524-475X.2012.00829.xArticlePubMedGoogle Scholar
- Oliveira KMC, Barker JH, Berezikov E, Pindur L, Kynigopoulos S, Eischen-Loges M, Han Z, Bhavsar MB, Henrich D, Leppik L (2019) Electrical stimulation shifts healing/scarring towards regeneration in a rat limb amputation model. Sci Rep 9(1):11433. https://doi.org/10.1038/s41598-019-47389-wArticleCASPubMedPubMed CentralGoogle Scholar
- Hu W, Wei X, Zhu L, Yin D, Wei A, Bi X, Liu T, Zhou G, Qiang Y, Sun X, Wen Z, Pan Y (2019) Enhancing proliferation and migration of fibroblast cells by electric stimulation based on triboelectric nanogenerator. Nano Energy 57:600–607. https://doi.org/10.1016/j.nanoen.2018.12.077ArticleCASGoogle Scholar
- Pollack GH (2003) The role of aqueous interfaces in the cell. Adv Colloid Interface Sci 103(2):173–196. https://doi.org/10.1016/S0001-8686(02)00095-7ArticleCASPubMedGoogle Scholar
- Pollack GH, Reitz FB (2001) Phase transitions and molecular motion in the cell. Cell Mol Biol 47(5):885–900 CASPubMedGoogle Scholar
- Kay AR (2017) How cells can control their size by pumping ions. Front Cell Dev Biol 5:41 ArticleGoogle Scholar
- Huang L, Cormie P, Messerli MA, Robinson KR (2009) The involvement of Ca 2+ and integrins in directional responses of zebrafish keratocytes to electric fields. J Cell Physiol 219(1):162–172. https://doi.org/10.1002/jcp.21660ArticleCASPubMedGoogle Scholar
- McLaughlin S, Poo MM (1981) The role of electro-osmosis in the electric-field-induced movement of charged macromolecules on the surfaces of cells. Biophys J 34(1):85–93. https://doi.org/10.1016/S0006-3495(81)84838-2ArticleCASPubMedPubMed CentralGoogle Scholar
- Andreev VP (2013) Cytoplasmic electric fields and electroosmosis: possible solution for the paradoxes of the intracellular transport of biomolecules. PLoS One 8(4):e61884. https://doi.org/10.1371/journal.pone.0061884ArticleCASPubMedPubMed CentralGoogle Scholar
- Schwartz L, da Veiga Moreira J, Jolicoeur M (2018) Physical forces modulate cell differentiation and proliferation processes. J Cell Mol Med 22(2):738–745. https://doi.org/10.1111/jcmm.13417ArticlePubMedGoogle Scholar
- Rico-Varela J, Ho D, Wan LQ (2018) In vitro microscale models for embryogenesis. Adv Biosyst 2(6):1700235. https://doi.org/10.1002/adbi.201700235ArticlePubMedPubMed CentralGoogle Scholar
- Gao R-C, Zhang X-D, Sun Y-H, Kamimura Y, Mogilner A, Devreotes PN, Zhao M (2011) Different roles of membrane potentials in electrotaxis and chemotaxis of dictyostelium cells. Eukaryot Cell 10(9):1251–1256. https://doi.org/10.1128/EC.05066-11ArticleCASPubMedPubMed CentralGoogle Scholar
- Nakajima K-I, Zhu K, Sun Y-H, Hegyi B, Zeng Q, Murphy CJ, Small JV, Chen-Izu Y, Izumiya Y, Penninger JM, Zhao M (2015) KCNJ15/Kir4.2 couples with polyamines to sense weak extracellular electric fields in galvanotaxis. Nat Commun 6:8532. https://doi.org/10.1038/ncomms9532ArticleCASPubMedPubMed CentralGoogle Scholar
- Humphries J, Xiong L, Liu J, Prindle A, Yuan F, Arjes HA, Tsimring L, Süel GM (2017) Species-independent attraction to biofilms through electrical signaling. Cell 168(1):200–9.e12. https://doi.org/10.1016/j.cell.2016.12.014ArticleCASPubMedPubMed CentralGoogle Scholar
- Borgens RB, Vanable JW Jr, Jaffe LF (1977) Bioelectricity and regeneration: large currents leave the stumps of regenerating newt limbs. Proc Natl Acad Sci USA 74(10):4528–4532. https://doi.org/10.1073/pnas.74.10.4528ArticleCASPubMedGoogle Scholar
- Franklin BM, Voss SR, Osborn JL (2017) Ion channel signaling influences cellular proliferation and phagocyte activity during axolotl tail regeneration. Mech Dev 146:42–54. https://doi.org/10.1016/j.mod.2017.06.001ArticleCASPubMedPubMed CentralGoogle Scholar
- Dahal GR, Pradhan SJ, Bates EA (2017) Inwardly rectifying potassium channels influence Drosophila wing morphogenesis by regulating Dpp release. Development (Cambridge, England) 144(15):2771–2783. https://doi.org/10.1242/dev.146647ArticleCASGoogle Scholar
- Sahu A, Ghosh R, Deshpande G, Prasad M (2017) A gap junction protein, Inx2, modulates calcium flux to specify border cell fate during Drosophila oogenesis. PLoS Genet 13(1):e1006542. https://doi.org/10.1371/journal.pgen.1006542ArticleCASPubMedPubMed CentralGoogle Scholar
- Richard M, Hoch M (2015) Drosophila eye size is determined by Innexin 2-dependent Decapentaplegic signalling. Dev Biol 408(1):26–40. https://doi.org/10.1016/j.ydbio.2015.10.011ArticleCASPubMedGoogle Scholar
- Bates EA (2013) A potential molecular target for morphological defects of fetal alcohol syndrome: Kir2.1. Curr Opin Genet Dev 23(3):324–329. https://doi.org/10.1016/j.gde.2013.05.001ArticleCASPubMedGoogle Scholar
- Bayir E, Sendemir A, Missirlis YF (2019) Mechanobiology of cells and cell systems, such as organoids. Biophys Rev. https://doi.org/10.1007/s12551-019-00590-7ArticlePubMedPubMed CentralGoogle Scholar
- Pannekoek W-J, de Rooij J, Gloerich M (2019) Force transduction by cadherin adhesions in morphogenesis. F1000 Res. 8:F1000. https://doi.org/10.12688/f1000research.18779.1ArticleGoogle Scholar
- Humphrey JD, Dufresne ER, Schwartz MA (2014) Mechanotransduction and extracellular matrix homeostasis. Nat Rev Mol Cell Biol 15:802. https://doi.org/10.1038/nrm3896ArticleCASPubMedPubMed CentralGoogle Scholar
- Li R, Baek KI, Chang CC, Zhou B, Hsiai TK (2019) Mechanosensitive pathways involved in cardiovascular development and homeostasis in zebrafish. J Vasc Res. https://doi.org/10.1159/000501883ArticlePubMedGoogle Scholar
- Finkelstein EI, Chao PH, Hung CT, Bulinski JC (2007) Electric field-induced polarization of charged cell surface proteins does not determine the direction of galvanotaxis. Cell Motil Cytoskelet 64(11):833–846. https://doi.org/10.1002/cm.20227ArticleCASGoogle Scholar
- Lin B-J, Tsao S-H, Chen A, Hu S-K, Chao L, Chao P-HG (2017) Lipid rafts sense and direct electric field-induced migration. Proc Natl Acad Sci USA 114(32):8568–8573. https://doi.org/10.1073/pnas.1702526114ArticleCASPubMedGoogle Scholar
- Zhu K, Takada Y, Nakajima K, Sun Y, Jiang J, Zhang Y, Zeng Q, Takada Y, Zhao M (2019) Expression of integrins to control migration direction of electrotaxis. FASEB J 33(8):9131–9141. https://doi.org/10.1096/fj.201802657RArticleCASPubMedPubMed CentralGoogle Scholar
- Casares D, Escribá PV, Rosselló CA (2019) Membrane lipid composition: effect on membrane and organelle structure, function and compartmentalization and therapeutic avenues. Int J Mol Sci 20(9):2167. https://doi.org/10.3390/ijms20092167ArticleCASPubMed CentralGoogle Scholar
- Allen Greg M, Mogilner A, Theriot Julie A (2013) Electrophoresis of cellular membrane components creates the directional cue guiding keratocyte galvanotaxis. Curr Biol 23(7):560–568. https://doi.org/10.1016/j.cub.2013.02.047ArticleCASPubMedPubMed CentralGoogle Scholar
- Forrester JV, Lois N, Zhao M, McCaig C (2007) The spark of life: the role of electric fields in regulating cell behaviour using the eye as a model system. Ophthalmic Res 39(1):4–16. https://doi.org/10.1159/000097901ArticlePubMedGoogle Scholar
- Mycielska ME, Djamgoz MBA (2004) Cellular mechanisms of direct-current electric field effects: galvanotaxis and metastatic disease. J Cell Sci 117(9):1631. https://doi.org/10.1242/jcs.01125ArticleCASPubMedGoogle Scholar
- Zhao MIN, Pu JIN, Forrester JV, McCaig CD (2002) Membrane lipids, EGF receptors, and intracellular signals colocalize and are polarized in epithelial cells moving directionally in a physiological electric field. FASEB J 16(8):857–859. https://doi.org/10.1096/fj.01-0811fjeArticleCASPubMedGoogle Scholar
- Fang KS, Ionides E, Oster G, Nuccitelli R, Isseroff RR (1999) Epidermal growth factor receptor relocalization and kinase activity are necessary for directional migration of keratinocytes in DC electric fields. J Cell Sci 112(12):1967 CASPubMedGoogle Scholar
- Reid B, Zhao M (2014) The electrical response to injury: molecular mechanisms and wound healing. Adv Wound Care (New Rochelle) 3(2):184–201. https://doi.org/10.1089/wound.2013.0442ArticleGoogle Scholar
- McLaughlin KA, Levin M (2018) Bioelectric signaling in regeneration: mechanisms of ionic controls of growth and form. Dev Biol 433(2):177–189. https://doi.org/10.1016/j.ydbio.2017.08.032ArticleCASPubMedGoogle Scholar
- Guo L, Li H, Wang Y, Li Z, Albeck J, Zhao M, Qing Q (2019) Controlling ERK activation dynamics in mammary epithelial cells with alternating electric fields through microelectrodes. Nano Lett 19(10):7526–7533. https://doi.org/10.1021/acs.nanolett.9b03411ArticleCASPubMedGoogle Scholar
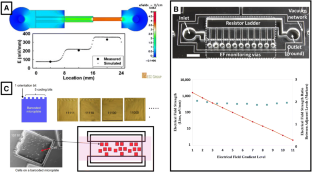
- Mobini S, Leppik L, Barker JH (2016) Direct current electrical stimulation chamber for treating cells in vitro. Biotechniques 60(2):95–98. https://doi.org/10.2144/000114382ArticleCASPubMedGoogle Scholar
- Mobini S, Leppik L, Thottakkattumana Parameswaran V, Barker JH (2017) In vitro effect of direct current electrical stimulation on rat mesenchymal stem cells. PeerJ 5:e2821. https://doi.org/10.7717/peerj.2821ArticleCASPubMedPubMed CentralGoogle Scholar
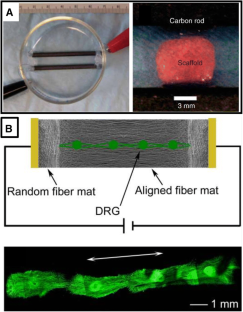
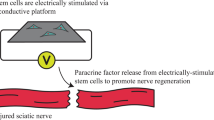
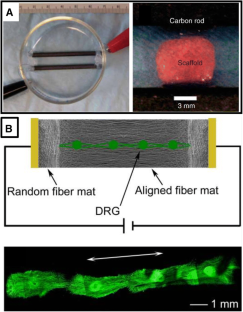
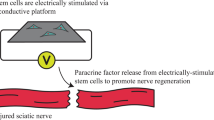
- Du J, Zhen G, Chen H, Zhang S, Qing L, Yang X, Lee G, Mao HQ, Jia X (2018) Optimal electrical stimulation boosts stem cell therapy in nerve regeneration. Biomaterials 181:347–359. https://doi.org/10.1016/j.biomaterials.2018.07.015ArticleCASPubMedPubMed CentralGoogle Scholar
- Wu SY, Hou HS, Sun YS, Cheng JY, Lo KY (2015) Correlation between cell migration and reactive oxygen species under electric field stimulation. Biomicrofluidics 9(5):054120. https://doi.org/10.1063/1.4932662ArticleCASPubMedPubMed CentralGoogle Scholar
- Huang CW, Cheng JY, Yen MH, Young TH (2009) Electrotaxis of lung cancer cells in a multiple-electric-field chip. Biosens Bioelectron 24(12):3510–3516. https://doi.org/10.1016/j.bios.2009.05.001ArticleCASPubMedGoogle Scholar
- Zhao S, Zhu K, Zhang Y, Zhu Z, Xu Z, Zhao M, Pan T (2014) ElectroTaxis-on-a-Chip (ETC): an integrated quantitative high-throughput screening platform for electrical field-directed cell migration. Lab Chip 14(22):4398–4405. https://doi.org/10.1039/c4lc00745jArticleCASPubMedPubMed CentralGoogle Scholar
- Tsai HF, Peng SW, Wu CY, Chang HF, Cheng JY (2012) Electrotaxis of oral squamous cell carcinoma cells in a multiple-electric-field chip with uniform flow field. Biomicrofluidics 6(3):34116. https://doi.org/10.1063/1.4749826ArticleCASPubMedGoogle Scholar
- Gao R, Zhao S, Jiang X, Sun Y, Zhao S, Gao J, Borleis J, Willard S, Tang M, Cai H, Kamimura Y, Huang Y, Jiang J, Huang Z, Mogilner A, Pan T, Devreotes PN, Zhao M (2015) A large-scale screen reveals genes that mediate electrotaxis in Dictyostelium discoideum. Sci Signal. 8(378):ra50. https://doi.org/10.1126/scisignal.aab0562ArticleCASPubMedPubMed CentralGoogle Scholar
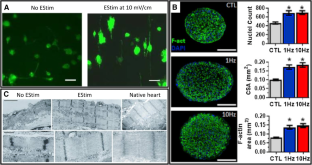
- Tandon N, Marsano A, Maidhof R, Wan L, Park H, Vunjak-Novakovic G (2011) Optimization of electrical stimulation parameters for cardiac tissue engineering. J Tissue Eng Regen Med 5(6):e115–e125. https://doi.org/10.1002/term.377ArticleCASPubMedPubMed CentralGoogle Scholar
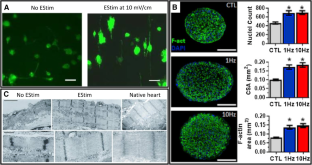
- Hirt MN, Boeddinghaus J, Mitchell A, Schaaf S, Bornchen C, Muller C, Schulz H, Hubner N, Stenzig J, Stoehr A, Neuber C, Eder A, Luther PK, Hansen A, Eschenhagen T (2014) Functional improvement and maturation of rat and human engineered heart tissue by chronic electrical stimulation. J Mol Cell Cardiol 74:151–161. https://doi.org/10.1016/j.yjmcc.2014.05.009ArticleCASPubMedGoogle Scholar
- Lasher RA, Pahnke AQ, Johnson JM, Sachse FB, Hitchcock RW (2012) Electrical stimulation directs engineered cardiac tissue to an age-matched native phenotype. J Tissue Eng 3(1):2041731412455354. https://doi.org/10.1177/2041731412455354ArticlePubMedPubMed CentralGoogle Scholar
- Ghasemi-Mobarakeh L, Prabhakaran MP, Morshed M, Nasr-Esfahani MH, Ramakrishna S (2009) Electrical stimulation of nerve cells using conductive nanofibrous scaffolds for nerve tissue engineering. Tissue Eng Part A 15(11):3605–3619. https://doi.org/10.1089/ten.TEA.2008.0689ArticleCASPubMedGoogle Scholar
- Xie J, Macewan MR, Willerth SM, Li X, Moran DW, Sakiyama-Elbert SE, Xia Y (2009) Conductive core-sheath nanofibers and their potential application in neural tissue engineering. Adv Funct Mater 19(14):2312–2318. https://doi.org/10.1002/adfm.200801904ArticleCASPubMedPubMed CentralGoogle Scholar
- Zhang Z, Rouabhia M, Wang Z, Roberge C, Shi G, Roche P, Li J, Dao LH (2007) Electrically conductive biodegradable polymer composite for nerve regeneration: electricity-stimulated neurite outgrowth and axon regeneration. Artif Organs 31(1):13–22. https://doi.org/10.1111/j.1525-1594.2007.00335.xArticleCASPubMedGoogle Scholar
- Lee JY, Bashur CA, Goldstein AS, Schmidt CE (2009) Polypyrrole-coated electrospun PLGA nanofibers for neural tissue applications. Biomaterials 30(26):4325–4335. https://doi.org/10.1016/j.biomaterials.2009.04.042ArticleCASPubMedPubMed CentralGoogle Scholar
- Huang J, Lu L, Zhang J, Hu X, Zhang Y, Liang W, Wu S, Luo Z (2012) Electrical stimulation to conductive scaffold promotes axonal regeneration and remyelination in a rat model of large nerve defect. PLoS One 7(6):e39526. https://doi.org/10.1371/journal.pone.0039526ArticleCASPubMedPubMed CentralGoogle Scholar
- Gordon T, Udina E, Verge VM, de Chaves EI (2009) Brief electrical stimulation accelerates axon regeneration in the peripheral nervous system and promotes sensory axon regeneration in the central nervous system. Motor Control 13(4):412–441 ArticleGoogle Scholar
- Xu C, Kou Y, Zhang P, Han N, Yin X, Deng J, Chen B, Jiang B (2014) Electrical stimulation promotes regeneration of defective peripheral nerves after delayed repair intervals lasting under one month. PLoS One 9(9):e105045. https://doi.org/10.1371/journal.pone.0105045ArticleCASPubMedPubMed CentralGoogle Scholar
- Banan Sadeghian R, Ebrahimi M, Salehi S (2018) Electrical stimulation of microengineered skeletal muscle tissue: effect of stimulus parameters on myotube contractility and maturation. J Tissue Eng Regen Med 12(4):912–922. https://doi.org/10.1002/term.2502ArticleCASPubMedGoogle Scholar
- Khodabukus A, Madden L, Prabhu NK, Koves TR, Jackman CP, Muoio DM, Bursac N (2019) Electrical stimulation increases hypertrophy and metabolic flux in tissue-engineered human skeletal muscle. Biomaterials 198:259–269. https://doi.org/10.1016/j.biomaterials.2018.08.058ArticleCASPubMedGoogle Scholar
- Ito A, Yamamoto Y, Sato M, Ikeda K, Yamamoto M, Fujita H, Nagamori E, Kawabe Y, Kamihira M (2014) Induction of functional tissue-engineered skeletal muscle constructs by defined electrical stimulation. Sci Rep 4:4781. https://doi.org/10.1038/srep04781ArticleCASPubMedPubMed CentralGoogle Scholar
- Radisic M, Park H, Shing H, Consi T, Schoen FJ, Langer R, Freed LE, Vunjak-Novakovic G (2004) Functional assembly of engineered myocardium by electrical stimulation of cardiac myocytes cultured on scaffolds. Proc Natl Acad Sci USA 101(52):18129–18134. https://doi.org/10.1073/pnas.0407817101ArticleCASPubMedGoogle Scholar
- Hu WW, Hsu YT, Cheng YC, Li C, Ruaan RC, Chien CC, Chung CA, Tsao CW (2014) Electrical stimulation to promote osteogenesis using conductive polypyrrole films. Mater Sci Eng C Mater Biol Appl 37:28–36. https://doi.org/10.1016/j.msec.2013.12.019ArticleCASPubMedGoogle Scholar
- Hu WW, Chen TC, Tsao CW, Cheng YC (2019) The effects of substrate-mediated electrical stimulation on the promotion of osteogenic differentiation and its optimization. J Biomed Mater Res B Appl Biomater 107(5):1607–1619. https://doi.org/10.1002/jbm.b.34253ArticleCASPubMedGoogle Scholar
- Tandon N, Cannizzaro C, Figallo E, Voldman J, Vunjak-Novakovic G (2006) Characterization of electrical stimulation electrodes for cardiac tissue engineering. Conf Proc IEEE Eng Med Biol Soc 1:845–848. https://doi.org/10.1109/IEMBS.2006.259747ArticleGoogle Scholar
- Balint R, Cassidy NJ, Cartmell SH (2014) Conductive polymers: towards a smart biomaterial for tissue engineering. Acta Biomater 10(6):2341–2353. https://doi.org/10.1016/j.actbio.2014.02.015ArticleCASPubMedGoogle Scholar
- Gorain B, Choudhury H, Pandey M, Kesharwani P, Abeer MM, Tekade RK, Hussain Z (2018) Carbon nanotube scaffolds as emerging nanoplatform for myocardial tissue regeneration: a review of recent developments and therapeutic implications. Biomed Pharmacother 104:496–508. https://doi.org/10.1016/j.biopha.2018.05.066ArticleCASPubMedGoogle Scholar
- Schmidt CE, Shastri VR, Vacanti JP, Langer R (1997) Stimulation of neurite outgrowth using an electrically conducting polymer. Proc Natl Acad Sci USA 94(17):8948–8953. https://doi.org/10.1073/pnas.94.17.8948ArticleCASPubMedGoogle Scholar
- Li M, Guo Y, Wei Y, MacDiarmid AG, Lelkes PI (2006) Electrospinning polyaniline-contained gelatin nanofibers for tissue engineering applications. Biomaterials 27(13):2705–2715. https://doi.org/10.1016/j.biomaterials.2005.11.037ArticleCASPubMedGoogle Scholar
- Chen MC, Sun YC, Chen YH (2013) Electrically conductive nanofibers with highly oriented structures and their potential application in skeletal muscle tissue engineering. Acta Biomater 9(3):5562–5572. https://doi.org/10.1016/j.actbio.2012.10.024ArticleCASPubMedGoogle Scholar
- Cen L, Neoh KG, Kang ET (2002) Surface functionalization of electrically conductive polypyrrole film with hyaluronic acid. Langmuir 18(22):8633–8640 ArticleCASGoogle Scholar
- Lee JW, Serna F, Nickels J, Schmidt CE (2006) Carboxylic acid-functionalized conductive polypyrrole as a bioactive platform for cell adhesion. Biomacromolecules 7(6):1692–1695. https://doi.org/10.1021/bm060220qArticleCASPubMedPubMed CentralGoogle Scholar
- Stauffer WR, Cui XT (2006) Polypyrrole doped with 2 peptide sequences from laminin. Biomaterials 27(11):2405–2413. https://doi.org/10.1016/j.biomaterials.2005.10.024ArticleCASPubMedGoogle Scholar
- Veetil JV, Ye K (2009) Tailored carbon nanotubes for tissue engineering applications. Biotechnol Prog 25(3):709–721. https://doi.org/10.1002/btpr.165ArticleCASPubMedPubMed CentralGoogle Scholar
- Mollon B, da Silva V, Busse JW, Einhorn TA, Bhandari M (2008) Electrical stimulation for long-bone fracture-healing: a meta-analysis of randomized controlled trials. J Bone Joint Surg Am 90(11):2322–2330. https://doi.org/10.2106/JBJS.H.00111ArticlePubMedGoogle Scholar
- Eberstein A, Eberstein S (1996) Electrical stimulation of denervated muscle: is it worthwhile? Med Sci Sports Exerc 28(12):1463–1469 ArticleCASGoogle Scholar
- Kern H, Hofer C, Strohhofer M, Mayr W, Richter W, Stohr H (1999) Standing up with denervated muscles in humans using functional electrical stimulation. Artif Organs 23(5):447–452. https://doi.org/10.1046/j.1525-1594.1999.06376.xArticleCASPubMedGoogle Scholar
- Mortimer JT, Bhadra N (2004) Peripheral nerve and muscle stimulation. In: Horch KW, Dhillon GS (eds) Series on bioengineering and biomedical engineering
- Cogan SF, Ludwig KA, Welle CG, Takmakov P (2016) Tissue damage thresholds during therapeutic electrical stimulation. J Neural Eng 13(2):021001. https://doi.org/10.1088/1741-2560/13/2/021001ArticlePubMedPubMed CentralGoogle Scholar
- Butterwick A, Vankov A, Huie P, Freyvert Y, Palanker D (2007) Tissue damage by pulsed electrical stimulation. IEEE Trans Biomed Eng 54(12):2261–2267. https://doi.org/10.1109/tbme.2007.908310ArticleCASPubMedGoogle Scholar
- Wong JN, Olson JL, Morhart MJ, Chan KM (2015) Electrical stimulation enhances sensory recovery: a randomized controlled trial. Ann Neurol. 77(6):996–1006. https://doi.org/10.1002/ana.24397ArticlePubMedGoogle Scholar
- Chan KM, Curran MW, Gordon T (2016) The use of brief post-surgical low frequency electrical stimulation to enhance nerve regeneration in clinical practice. J Physiol 594(13):3553–3559. https://doi.org/10.1113/JP270892ArticleCASPubMedPubMed CentralGoogle Scholar
- Vance CG, Dailey DL, Rakel BA, Sluka KA (2014) Using TENS for pain control: the state of the evidence. Pain Manag 4(3):197–209. https://doi.org/10.2217/pmt.14.13ArticlePubMedPubMed CentralGoogle Scholar
- Guo X, Jiang X, Ren X, Sun H, Zhang D, Zhang Q, Zhang J, Huang Y (2015) The galvanotactic migration of keratinocytes is enhanced by hypoxic preconditioning. Sci Rep 5:10289. https://doi.org/10.1038/srep10289ArticleCASPubMedPubMed CentralGoogle Scholar
- Ren X, Sun H, Liu J, Guo X, Huang J, Jiang X, Zhang Y, Huang Y, Fan D, Zhang J (2019) Keratinocyte electrotaxis induced by physiological pulsed direct current electric fields. Bioelectrochemistry 127:113–124. https://doi.org/10.1016/j.bioelechem.2019.02.001ArticleCASPubMedGoogle Scholar
- Kim MS, Lee MH, Kwon BJ, Seo HJ, Koo MA, You KE, Kim D, Park JC (2017) Control of neonatal human dermal fibroblast migration on poly(lactic-co-glycolic acid)-coated surfaces by electrotaxis. J Tissue Eng Regen Med 11(3):862–868. https://doi.org/10.1002/term.1986ArticleCASPubMedGoogle Scholar
- Guo A, Song B, Reid B, Gu Y, Forrester JV, Jahoda CA, Zhao M (2010) Effects of physiological electric fields on migration of human dermal fibroblasts. J Investig Dermatol 130(9):2320–2327. https://doi.org/10.1038/jid.2010.96ArticleCASPubMedGoogle Scholar
- Peters EJ, Lavery LA, Armstrong DG, Fleischli JG (2001) Electric stimulation as an adjunct to heal diabetic foot ulcers: a randomized clinical trial. Arch Phys Med Rehabil 82(6):721–725. https://doi.org/10.1053/apmr.2001.23780ArticleCASPubMedGoogle Scholar
- Wood JM, Evans PE 3rd, Schallreuter KU, Jacobson WE, Sufit R, Newman J, White C, Jacobson M (1993) A multicenter study on the use of pulsed low-intensity direct current for healing chronic stage II and stage III decubitus ulcers. Arch Dermatol 129(8):999–1009 ArticleCASGoogle Scholar
- Houghton PE, Campbell KE, Fraser CH, Harris C, Keast DH, Potter PJ, Hayes KC, Woodbury MG (2010) Electrical stimulation therapy increases rate of healing of pressure ulcers in community-dwelling people with spinal cord injury. Arch Phys Med Rehabil 91(5):669–678. https://doi.org/10.1016/j.apmr.2009.12.026ArticlePubMedGoogle Scholar
- Griffin JW, Tooms RE, Mendius RA, Clifft JK, Vander Zwaag R, El-Zeky F (1991) Efficacy of high voltage pulsed current for healing of pressure ulcers in patients with spinal cord injury. Phys Ther 71(6):433–444. https://doi.org/10.1093/ptj/71.6.433(discussion 42–4)ArticleCASPubMedGoogle Scholar
- Houghton PE, Kincaid CB, Lovell M, Campbell KE, Keast DH, Woodbury MG, Harris KA (2003) Effect of electrical stimulation on chronic leg ulcer size and appearance. Phys Ther 83(1):17–28 ArticleGoogle Scholar
- Adunsky A, Ohry A, Group D (2005) Decubitus direct current treatment (DDCT) of pressure ulcers: results of a randomized double-blinded placebo controlled study. Arch Gerontol Geriatr 41(3):261–269. https://doi.org/10.1016/j.archger.2005.04.004ArticlePubMedGoogle Scholar
- Lundeberg TC, Eriksson SV, Malm M (1992) Electrical nerve stimulation improves healing of diabetic ulcers. Ann Plast Surg 29(4):328–331 ArticleCASGoogle Scholar
- Carley PJ, Wainapel SF (1985) Electrotherapy for acceleration of wound healing: low intensity direct current. Arch Phys Med Rehabil 66(7):443–446 CASPubMedGoogle Scholar
- Jankovic A, Binic I (2008) Frequency rhythmic electrical modulation system in the treatment of chronic painful leg ulcers. Arch Dermatol Res 300(7):377–383. https://doi.org/10.1007/s00403-008-0875-9ArticlePubMedGoogle Scholar
- Lawson D, Petrofsky JS (2007) A randomized control study on the effect of biphasic electrical stimulation in a warm room on skin blood flow and healing rates in chronic wounds of patients with and without diabetes. Med Sci Monit 13(6):CR258–CR263 PubMedGoogle Scholar
- Feedar JA, Kloth LC, Gentzkow GD (1991) Chronic dermal ulcer healing enhanced with monophasic pulsed electrical stimulation. Phys Ther 71(9):639–649. https://doi.org/10.1093/ptj/71.9.639ArticleCASPubMedGoogle Scholar
- Morris C (2006) Bio-electrical stimulation therapy using POSiFECT ® RD. Wounds UK 2(4):112–116 Google Scholar
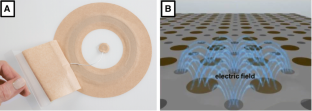
- Banerjee J, Das Ghatak P, Roy S, Khanna S, Sequin EK, Bellman K, Dickinson BC, Suri P, Subramaniam VV, Chang CJ, Sen CK (2014) Improvement of human keratinocyte migration by a redox active bioelectric dressing. PLoS One 9(3):e89239. https://doi.org/10.1371/journal.pone.0089239ArticleCASPubMedPubMed CentralGoogle Scholar
- Kim H, Makin I, Skiba J, Ho A, Housler G, Stojadinovic A, Izadjoo M (2014) Antibacterial efficacy testing of a bioelectric wound dressing against clinical wound pathogens. Open Microbiol J 8:15–21. https://doi.org/10.2174/1874285801408010015ArticleCASPubMedPubMed CentralGoogle Scholar
- Leloup P, Toussaint P, Lembelembe JP, Celerier P, Maillard H (2015) The analgesic effect of electrostimulation (WoundEL(R)) in the treatment of leg ulcers. Int Wound J 12(6):706–709. https://doi.org/10.1111/iwj.12211ArticlePubMedGoogle Scholar
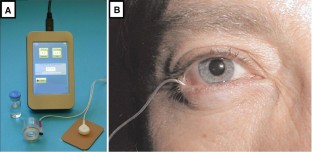
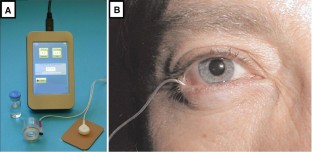
- Zhang Y, Chen Y, Yu X, Qi Y, Chen Y, Liu Y, Hu Y, Li Z (2016) A flexible device for ocular iontophoretic drug delivery. Biomicrofluidics 10(1):011911. https://doi.org/10.1063/1.4942516ArticleCASPubMedPubMed CentralGoogle Scholar
- Jung JH, Chiang B, Grossniklaus HE, Prausnitz MR (2018) Ocular drug delivery targeted by iontophoresis in the suprachoroidal space using a microneedle. J Control Release 277:14–22. https://doi.org/10.1016/j.jconrel.2018.03.001ArticleCASPubMedPubMed CentralGoogle Scholar
- Christopher K, Chauhan A (2019) Contact lens based drug delivery to the posterior segment via iontophoresis in cadaver rabbit eyes. Pharm Res 36(6):87. https://doi.org/10.1007/s11095-019-2625-4ArticleCASPubMedGoogle Scholar
- O’Brart DP (2016) Riboflavin for corneal cross-linking. Drugs Today (Barc) 52(6):331–346. https://doi.org/10.1358/dot.2016.52.6.2494140ArticleGoogle Scholar
- Bikbova G, Bikbov M (2014) Transepithelial corneal collagen cross-linking by iontophoresis of riboflavin. Acta Ophthalmol 92(1):e30–e34. https://doi.org/10.1111/aos.12235ArticleCASPubMedGoogle Scholar
- Bikbova G, Bikbov M (2016) Standard corneal collagen crosslinking versus transepithelial iontophoresis-assisted corneal crosslinking, 24 months follow-up: randomized control trial. Acta Ophthalmol 94(7):e600–e606. https://doi.org/10.1111/aos.13032ArticleCASPubMedPubMed CentralGoogle Scholar
- Patane MA, Cohen A, From S, Torkildsen G, Welch D, Ousler GW 3rd (2011) Ocular iontophoresis of EGP-437 (dexamethasone phosphate) in dry eye patients: results of a randomized clinical trial. Clin Ophthalmol 5:633–643. https://doi.org/10.2147/OPTH.S19349ArticleCASPubMedPubMed CentralGoogle Scholar
- Cohen AE, Assang C, Patane MA, From S, Korenfeld M, Avion Study I (2012) Evaluation of dexamethasone phosphate delivered by ocular iontophoresis for treating noninfectious anterior uveitis. Ophthalmology 119(1):66–73. https://doi.org/10.1016/j.ophtha.2011.07.006ArticlePubMedGoogle Scholar
- Halhal M, Renard G, Courtois Y, BenEzra D, Behar-Cohen F (2004) Iontophoresis: from the lab to the bed side. Exp Eye Res 78(3):751–757 ArticleCASGoogle Scholar
- Haghjou N, Soheilian M, Abdekhodaie MJ (2011) Sustained release intraocular drug delivery devices for treatment of uveitis. J Ophthalmic Vis Res 6(4):317–329 CASPubMedPubMed CentralGoogle Scholar
- Parkinson TM, Ferguson E, Febbraro S, Bakhtyari A, King M, Mundasad M (2003) Tolerance of ocular iontophoresis in healthy volunteers. J Ocul Pharmacol Ther 19(2):145–151. https://doi.org/10.1089/108076803321637672ArticleCASPubMedGoogle Scholar
- Churchill CDM, Winter P, Tuszynski JA, Levin M (2019) EDEn–electroceutical design environment: ion channel tissue expression database with small molecule modulators. iScience 11:42–56. https://doi.org/10.1016/j.isci.2018.12.003ArticleCASPubMedGoogle Scholar
- Fricke H (1953) The electric permittivity of a dilute suspension of membrane-covered ellipsoids. J Appl Phys 24(5):644–646. https://doi.org/10.1063/1.1721343ArticleCASGoogle Scholar
- Schwan HP (1957) Electrical properties of tissue and cell suspensions. In: Lawrence JH, Tobias CA (eds) Advances in biological and medical physics. Elsevier, Amsterdam, pp 147–209 Google Scholar
- Meny I, Burais N, Buret F, Nicolas L (2007) Finite-element modeling of cell exposed to harmonic and transient electric fields. IEEE Trans Magn 43(4):1773–1776. https://doi.org/10.1109/TMAG.2007.892517ArticleGoogle Scholar
- Gowrishankar TR, Smith KC, Weaver JC (2013) Transport-based biophysical system models of cells for quantitatively describing responses to electric fields. Proc IEEE 101(2):505–517. https://doi.org/10.1109/JPROC.2012.2200289ArticleGoogle Scholar
- Schoenbach KH, Joshi RP, Kolb JF, Nianyong C, Stacey M, Blackmore PF, Buescher ES, Beebe SJ (2004) Ultrashort electrical pulses open a new gateway into biological cells. Proc IEEE 92(7):1122–1137. https://doi.org/10.1109/JPROC.2004.829009ArticleCASGoogle Scholar
- Pietak A, Levin M (2016) Exploring instructive physiological signaling with the bioelectric tissue simulation engine. Front Bioeng Biotechnol 4:55. https://doi.org/10.3389/fbioe.2016.00055ArticlePubMedPubMed CentralGoogle Scholar
- Newbold C, Richardson R, Millard R, Seligman P, Cowan R, Shepherd R (2011) Electrical stimulation causes rapid changes in electrode impedance of cell-covered electrodes. J Neural Eng 8(3):036029. https://doi.org/10.1088/1741-2560/8/3/036029ArticlePubMedPubMed CentralGoogle Scholar
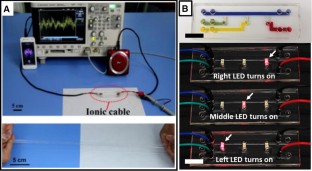
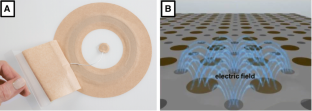
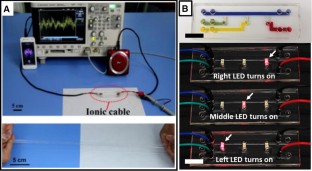
- Keplinger C, Sun JY, Foo CC, Rothemund P, Whitesides GM, Suo Z (2013) Stretchable, transparent, ionic conductors. Science 341(6149):984–987. https://doi.org/10.1126/science.1240228ArticleCASPubMedGoogle Scholar
- Sun JY, Keplinger C, Whitesides GM, Suo Z (2014) Ionic skin. Adv Mater 26(45):7608–7614. https://doi.org/10.1002/adma.201403441ArticleCASPubMedGoogle Scholar
- Yang CH, Chen B, Lu JJ, Yang JH, Zhou J, Chen YM, Suo Z (2015) Ionic cable. Extreme Mech Lett 3:59–65 ArticleGoogle Scholar
- Kim CC, Lee HH, Oh KH, Sun JY (2016) Highly stretchable, transparent ionic touch panel. Science 353(6300):682–687. https://doi.org/10.1126/science.aaf8810ArticleCASPubMedGoogle Scholar
- Zhao S, Tseng P, Grasman J, Wang Y, Li W, Napier B, Yavuz B, Chen Y, Howell L, Rincon J, Omenetto FG, Kaplan DL (2018) Programmable hydrogel ionic circuits for biologically matched electronic interfaces. Adv Mater 30(25):e1800598. https://doi.org/10.1002/adma.201800598ArticleCASPubMedGoogle Scholar
Acknowledgements
S. Zhao thanks the Research Start-Up Funds from the University of Nebraska Medical Center for support of this work. The work in M. Zhao lab was supported by National Institutes of Health (NIH), National Eye Institute Grant EY019101, U.S. Air Force Office of Scientific Research (AFOSR) Multidisciplinary University Research Initiatives (MURI) Grant FA9550-16-1-0052, and Karen Burns Cornea Research fund. National Institute on Aging grant R21AG060335, NEI core grant P-30 EY012576, and unrestricted grant from Research to Prevent Blindness, Inc.